Last month, the International Training and Education Center for Health (I-TECH), in collaboration with the U.S. Centers for Disease Control (CDC) and with support from the World Health Organization (WHO), facilitated the second of three in-person workshops for the Informatics and Data Science for Health (IDASH) fellowship.
Held in Almaty, Kazakhstan, the workshop marked the mid-point of the 12-month fellowship—and a chance for participants to come together to advance their ability to apply public health informatics and data science concepts and approaches.
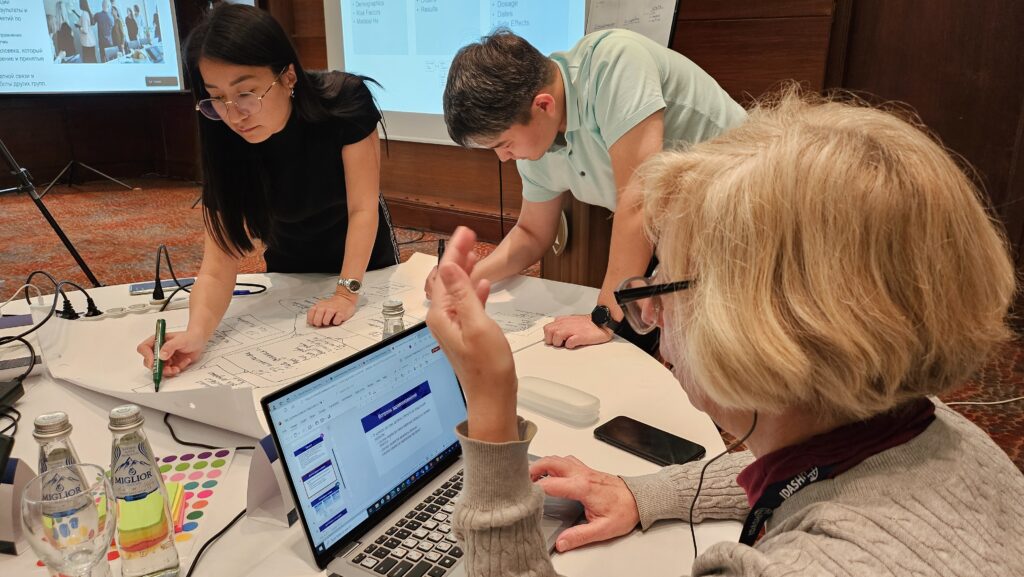
“This workshop included a lot of hands-on practical exercises, and it was fun to observe how engaged the participants were with these activities and with the learning in general,” said Stacey Lissit, MPH, MS, Senior Technical Advisor for the IDASH program.
Content included all things data (quality, cleaning, analysis, visualization, governance, security, privacy, and confidentiality); interoperability; project management; business process analysis; and systems architecture. Sessions were a mix of didactic lecture, small group activities to practice application of skills and concepts, peer feedback, and guided hands-on learning in R and PowerBI. Over the course of the two weeks, participants collaborated to develop a data dashboard, a database schema, and a data quality workplan.

The current fellowship, launched in April 2023, comprises a cohort of four participants each from Georgia, Kazakhstan, Kyrgyzstan, Ukraine, and Uzbekistan—a total of 20 fellows. Each four-person team includes a mix of mid-senior level epidemiologists, informaticians, data scientists, IT, and public health policy personnel.
Fellow Zhanibek Yerubayev, Director of Public Health Emergency Operations at the Kazakhstan Ministry of Health’s National Center of Public Health, says the team mix is an integral part of IDASH’s impact. “[IDASH] connects people from the public health side with people from the IT side,” he says. “These people have a lot of projects to do [together], but they are not always well connected, and they do not always understand each other well.”
“It was exciting to see the relationships and community that are being built through the IDASH Fellowship – both within the country teams where fellows can collaborate closely with colleagues outside of their typical ‘work silos,’ and across countries within the region,” said Lissit. “That peer learning element is such an important part of the fellowship.”
And all efforts were made to ensure multi-directional collaboration. The Ukrainian team did not receive permission to travel to the workshop, so I-TECH made arrangements for them to participate via Zoom. A location was identified in southwest Ukraine where the team could attend the workshop together remotely, experience fewer daily safety issues related to the war, and avoid the distractions of being in their own workplace. A simultaneous translator for the Ukrainian language was provided on the Zoom call.
While remote participation is not ideal, the Ukraine team was able to attend and hear most of the workshop sessions and engage in the group work in meaningful ways. “A lot of effort went into setting up the technology that enabled this participation,” said Lissit. “At one point the Ukraine team was participating in a peer feedback activity with two country teams in Almaty—there were live cameramen, screen sharing, Zoom translators…and it worked mostly seamlessly!”
Fellow Durbek Aliyev, Deputy CEO at IT-Med LLC, which works under the Uzbekistan Ministry of Health, was especially appreciative of the chance to learn from a wide range experts across the region. “The digitalization of health care cannot be done by only one country itself,” said Aliyev. “The advantage of IDASH over other programs is that it brings [together] specialists from neighbor countries. We are talking to each other….We are learning from each other directly.”
And these relationships will be a lasting benefit of the program, he continued. “IDASH is a place where we can establish very good networking with other countries,” said Aliyev. “Any time I can contact them and learn from their expertise.”
IDASH is a project within the Integrated Next-Generation Surveillance in Global Health: Translation to Action (INSIGHT) program. In addition to acquiring new skills and knowledge in public health informatics and data science, IDASH country teams are developing and will implement a collaborative team project that demonstrates key competencies and is aligned with their country’s needs and priorities.